The bad Parts.
Whether you are seeing a gastroenterologist for the first time, or you’re already a Crohn’s patient and keeping up with your checkups, it’s important to prepare for your appointment by tracking your symptoms and writing down any questions you may have.
In general, there are two reasons to undergo Crohn’s tests and procedures:
To determine whether you have Crohn’s (to obtain or disprove a Crohn’s disease diagnosis)
To re-evaluate your Crohn’s disease — something your gastroenterologist will probably want to do on an ongoing, regular basis.
Common tests for Crohn’s disease are:
Blood Tests

Although blood tests alone cannot diagnose Crohn’s disease, they’re an important tool in diagnosis and monitoring of this disease. Several different kinds of blood tests are used.
Routine blood tests .
These are used to detect infection, anemia, indicators of inflammation, and to identify deficiencies of vitamins or minerals.
Fecal blood test
This is conducted to detect blood in your stool (with a stool sample), an indicator of bleeding in the intestines. It also helps rule out other causes of gastrointestinal diseases, such as infection. Your doctor will give you a container for collecting and storing the stool.
Antibody blood tests
These tests help your doctor determine whether you have Crohn’s or UC. They look for antibodies, proteins produced by the immune system that indicate the presence of one disease or the other. These tests, however, are not conclusive by themselves. A positive finding doesn’t mean you have Crohn’s, and a negative finding doesn’t mean that you don’t have it.
Imaging Tests.

These are tests that take pictures of different parts of your body to provide a clearer picture of your condition. They show your doctor areas of disease activity and identify possible complications. These are only some of the imaging tests used for Crohn’s—there are others your doctor may recommend.
Conventional X-rays.

A standard X-ray of your abdominal area can show narrowing of the intestines or an intestinal blockage, possibly from inflammation or scarring. It may also be done to rule out certain Crohn’s complications.
Contrast X-rays.
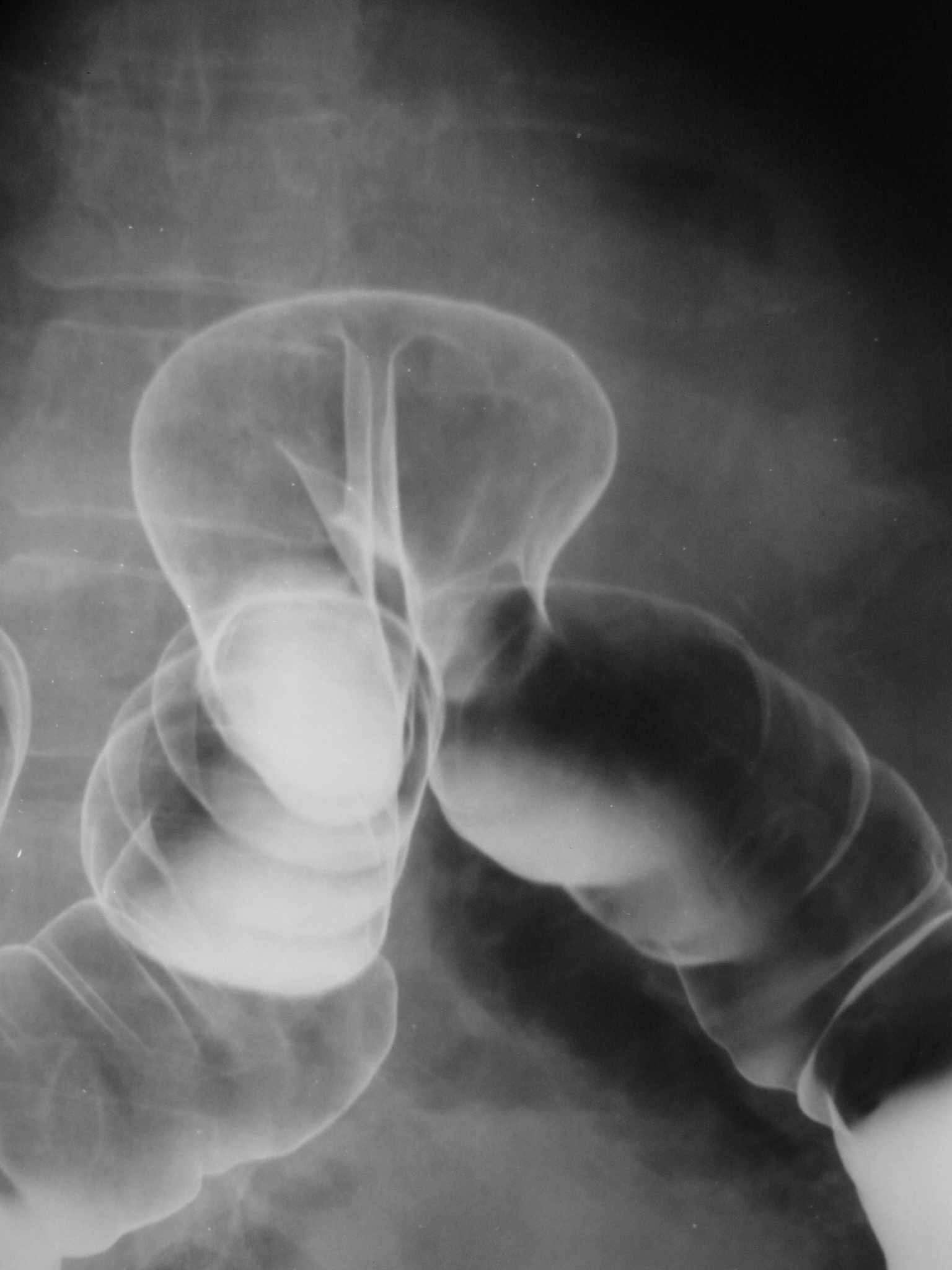
This diagnostic test allows your doctor to evaluate your intestine by tracking the movement of a thick, chalky liquid called barium. The barium dye coats the lining of the bowel, creating a silhouette of your rectum, colon, and a portion of your intestine that’s visible on an X-ray.
Computerized tomography (CT scan).

A CT scan takes simultaneous X-rays from different angles to create a cross-sectional image of the bowel, as well as images of tissues outside the bowel that can’t be seen with other tests. CT scans help your doctor to diagnose your Crohn’s and determine the location and extent of your disease. They can also help check for potential complications and rule out conditions with similar symptoms, such as appendicitis.
Leukocyte scintigraphy (white blood cell scan).

White blood cells are drawn to the site of inflammation in the body. This test tracks your white blood cells to determine how much inflammation Crohn’s may be causing in your gastrointestinal tract.
Endoscopy (includes colonoscopy). 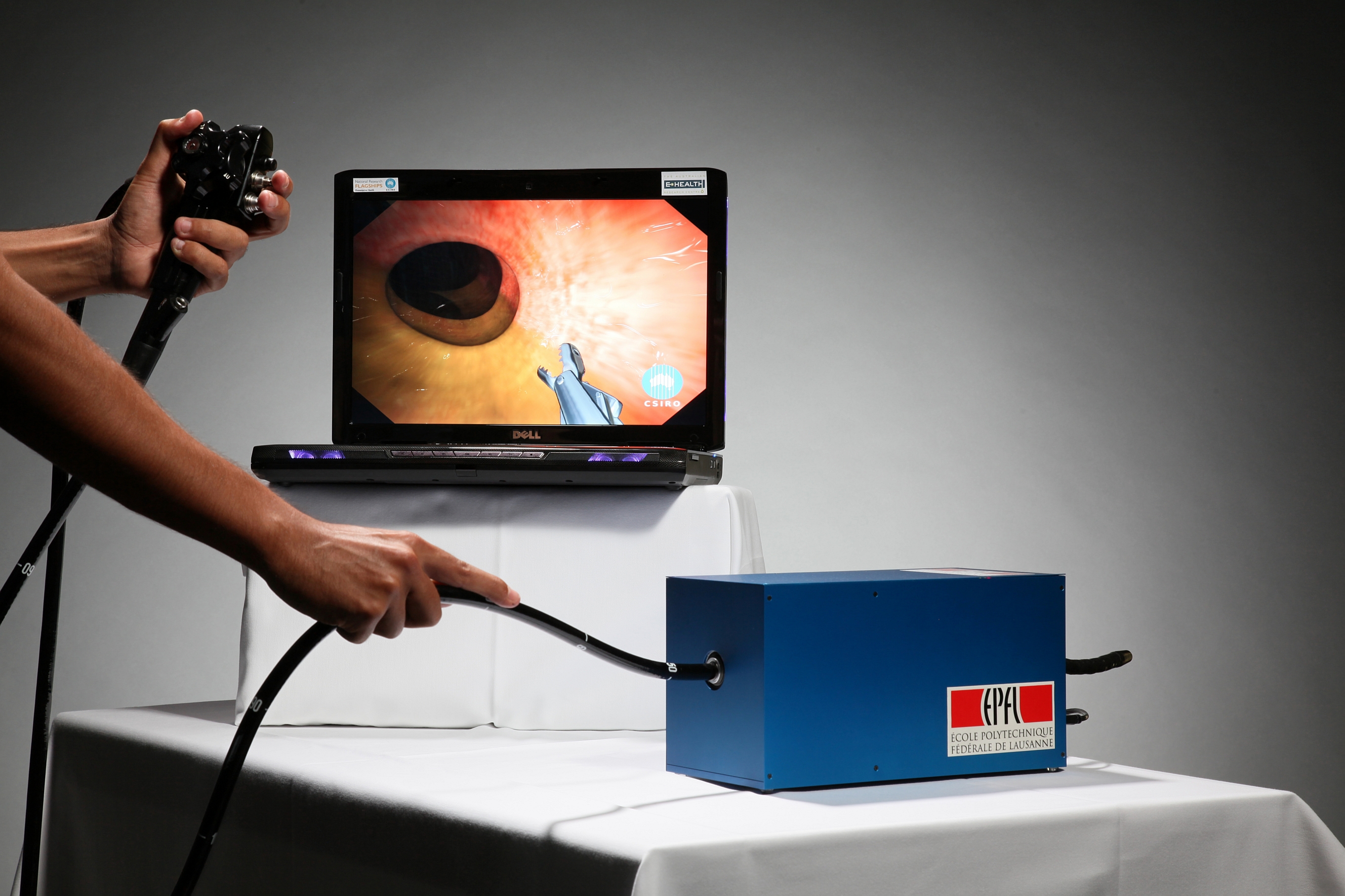
This test uses a thin, flexible tube with a lighted camera inside the tip (called an endoscope) that allows your doctor to explore the different parts of your GI tract. This technique includes tests such as:
Sigmoidoscopy: Examines the sigmoid, the lower third of your large intestine (the rectum and sigmoid colon).
Colonoscopy: Provides a view of your entire colon, and helps your doctor determine whether you have Crohn’s or UC.
Capsule endoscopy: Uses a tiny camera that you swallow in a capsule. The camera takes as many as 50,000 images, which are transmitted to a computer. Your doctor then downloads the images onto a monitor to check for signs of Crohn’s disease. Once it has gone through your digestive tract, the camera is passed painlessly in your stool.
Esophagogastroduodenoscopy (EGD): Also referred to as upper gastrointestinal (GI) endoscopy, examines 3 areas that can be affected by Crohn’s disease: the esophagus, the stomach, and the duodenum (the first part of the small intestine).
Endoscopic retrograde cholangiopancreatography (ERCP): This procedure combines upper gastrointestinal (GI) endoscopy and X-rays to examine bile ducts in the liver and pancreatic ducts, which may be affected in some people with Crohn’s.
Double-balloon endoscopy: A longer scope with 2 inflatable balloons attached is used to explore areas of the small bowel where standard endoscopes are unable to reach.
Endoscopic ultrasound.

This technique attaches an ultrasound probe to an endoscope to examine deep below the lining of the intestines. It is most often used to look at fistulae in the rectal area, a complication of Crohn’s disease.
Magnetic resonance imaging (MRI).
Large, tube-shaped magnets use a magnetic field and radio waves to create images. MRI is very helpful in diagnosing and managing Crohn’s.
Pelvic MRI.

Commonly used for evaluating fistula around the anal area.
MRI enterography: Commonly used for examining the small intestine.
This information was taken from Crohn`s and Colitis.com
